Case Report
The forgotten player in the surgical history

Yves Cirotteau*
Neuilly Sur Seine Hospital, Courbevoie, France
*Address for Correspondence: Yves Cirotteau, Neuilly Sur Seine Hospital, Courbevoie, France, Tel: +33O621888265; Email: [email protected]
Dates: Submitted: 12 February 2019; Approved: 10 May 2019; Published: 13 May 2019
How to cite this article:Cirotteau Y. The forgotten player in the surgical history . Int J Bone Marrow Res. 2019; 2: 051-063. DOI: 10.29328/journal.ijbmr.1001005
Copyright License: © 2019 Cirotteau Y. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The research concerning a preventive treatment of an osteoporitic femoral neck fracture started in 1990 because the surgical procedure of unstable femoral neck fractures is difficult. After effects are frequent and their number will increase in the next decade. The goal is to reinforce the femur with a biomaterial acting as a bone graft.
Natural coral is bioresorbable and biocompatible. It acts as an autofocus bone graft for reconstruction of either cortex or cancellous bone and increases their mechanical resistance.
This work shows evidence of new bone formation in an osteoporotic unbroken femoral neck femur. Consequently, the preventive surgical treatment of osteoporosis should be taken in consideration [1]. The purpose of this work is to show the results on the mineralization of the cancellous bone of an upper femoral metaphyses when a natural biomaterial is set in an unbroken osteoporotic femoral neck.
Summary: Mrs. L is an 84 years old lady. Her osteoporotic unbroken right hip was grafted preventively with a biomaterial in order to prevent the high risk of break in case of fall. The biomaterial used is beads of natural coral. The reasons of this preventive treatment is discussed, as well as the choice of the biomaterial. The results are shown including a two years follow up.
Brief History: Before going further, few words of history. Three centuries BC, an Aristote’s follower, Théophraste thinks that Natural coral is a petrified plant.
For Ovide natural coral is a soft alga air-hardening.
Al Biruni classes it among animals, because that respond to touch.
At the beginning of the XVIIth century, Marsigli thinks that they are flowers which open out there in aquarium.
The French Jean-André Peyssonnel, a young naturalist, says as Biruni, that in fact, corals are animals.
At last, Buffon claims: These marine plants, were classified first in the rank of minerals, then in those of plants, and finally in that of animals.
Natural coral is obviously an animal.
After the Second World War, coral samples were analyzed by American scientists. Among 800 corail species, 3 where specially analyzed: Acropora, Porites and Libophylia.
Mrs Nane Guillemin did in France her PHD on natural coral and with her team made a complete fundamental analysis (physical, chemical and biological properties) of the material, while the American scientists worked on the chemical bone’s properties.
In France, Pr Ohayoun and his team worked on the surgical application in the dental field, Dr. Yves Cirotteau in the orthopedic surgery, specifically for osteoporotic disease and for the traumatologic field
Clinical Story
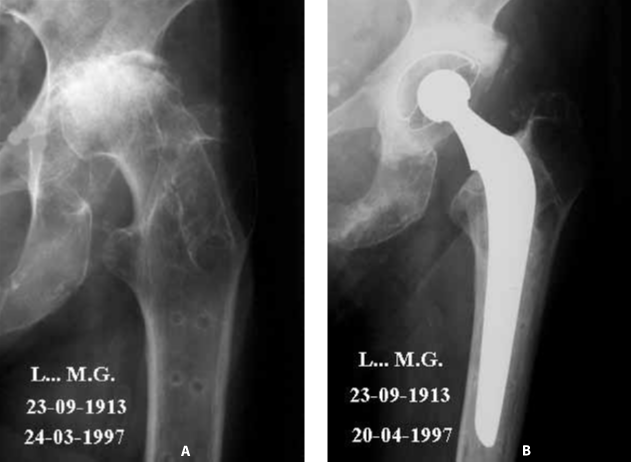
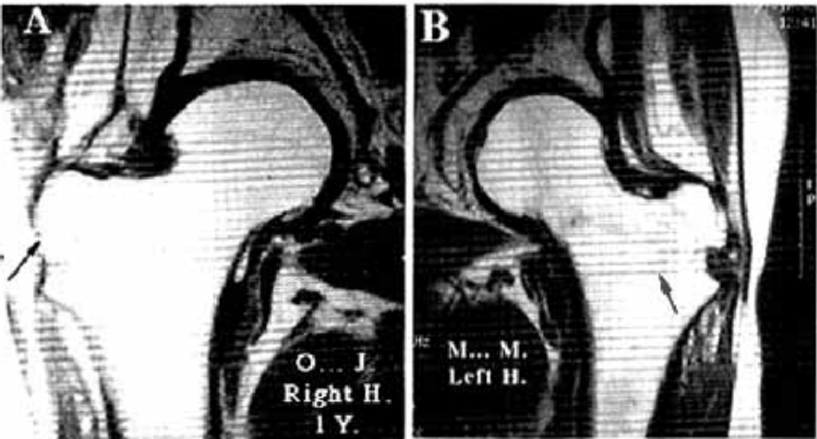
She is a cute little granny (1m48), 85 years old. She fractured her left hip. Secondary arthrosis resulted in the ablation of material (Figure 1AB).
The left hip arthrosis was so extended that she could no longer leave her home because of the pain. Being very active and alert, she highly suffered from this situation. The solution – for the left hip – was clearly a full prosthesis [2].
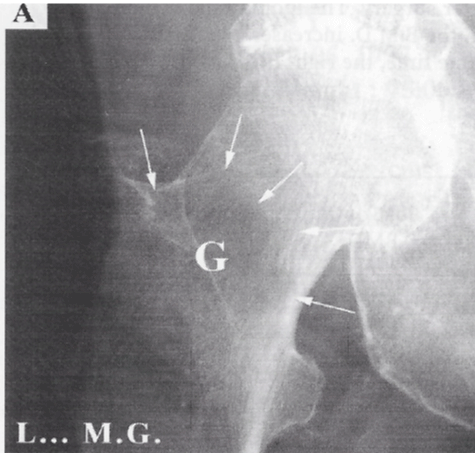
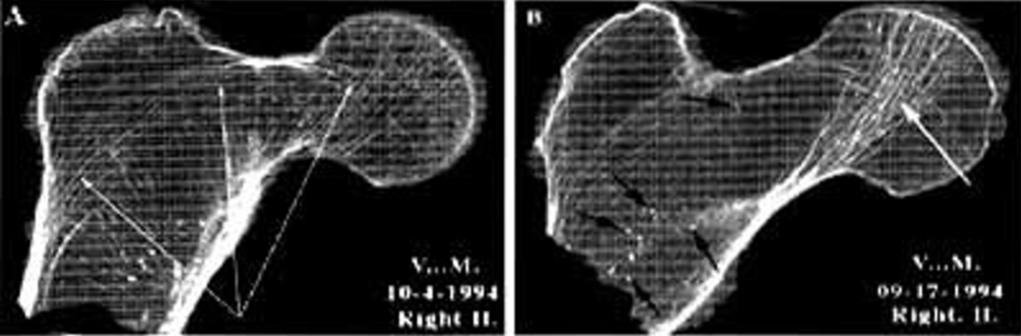
When looking carefully at the X-ray of the opposite hip, a large hole can be seen, its size and volume affecting the entire upper part of the femur. Not only the bone trabeculae was affected, but the whole bone was affected with hypodensity (Figure 2A).
It resulted in a huge hole in the right upper femoral metaphysis.
Osteodensitometry
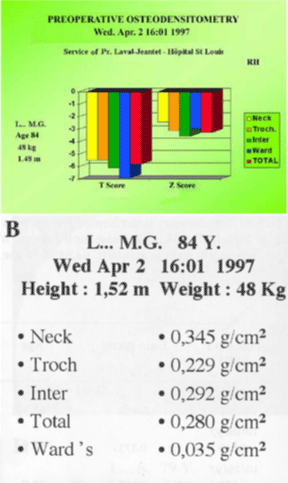
Two indexes have been defined to distinguish physiological osteopenia from osteoporotic disease: - The T-score measures bone mineral quantity at its highest level. This is the quantity found at a bone site in a young person.
The Z-score measures bone mineral quantity of the subject examined compared to a subject of the same age.
The osteoporotic disease is defined as a bone loss, 2,5 standard deviation below the value observed in a normal twenty years old adult.
Global loss – whether from the envelope or the content – can therefore reach 50, 60 and up to 90% of the maximum value.
The fracture threshold is the quantity of bone remaining, below which there is a high risk of fracture in the event of a fall [3,4]. For the hip, the threshold is 0.600 g/cm². The lower the threshold, the greater the theoretical risk of fracture.
Four areas are examined in the upper femoral metaphysis:
− The greater trochanter
− The intertrochanteric zone
− The femoral neck
− The Ward’s triangle
Bone densitometry in the affected part was only a few dozen mg/cm² (normally several hundred). It confirmed the severity of the osteoporosis.
Mrs L. MG: Osteodensitometry (10)
The osseous demineralisation is confirmed by the osteodensitometry. Note the very poor quantity of cancellous bone left in the Ward’s triangle: 0,035 g/cm2 (Figure 2B).
Under such conditions of bone fragility, the slightest fall was likely to induce a fracture. As the risk of fracture is more serious when densitometric loss is severe. Even worse, there was a very high risk of fatigue fracture that could occur simply during a longer than usual walk.
For example: you can break a thin metal wall with a sharp blow against a harder surface. This same wall can also be bent by bending it and moving it backwards and forwards. After several flexions the wall will suddenly break. This is a fatigue fracture [8].
After surgery with a full prosthesis, the patient may be fully active again thanks to suppression of pain [5]. Knowing that the other hip could be fractured at any moment, are we allowed to do nothing and wait for the fracture?
Neither from a moral nor a scientific point of view we should leave it at risk knowing the inevitable will happen sooner or later. When 85 years old you no longer have much life left ahead of you and later can arrive pretty soon. Also a second point of interests for trauma surgeons: the lower the bone densitometry is, the more complex the fracture is, the more difficult will be the surgical stabilization [6].
During a family reunion, the reasons for preventive treatment were explained. The family accepted the conclusions and a filling-graft was performed.
Surgical Technic
Osteoscopy (3)
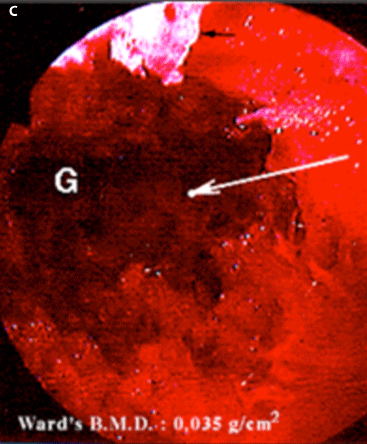
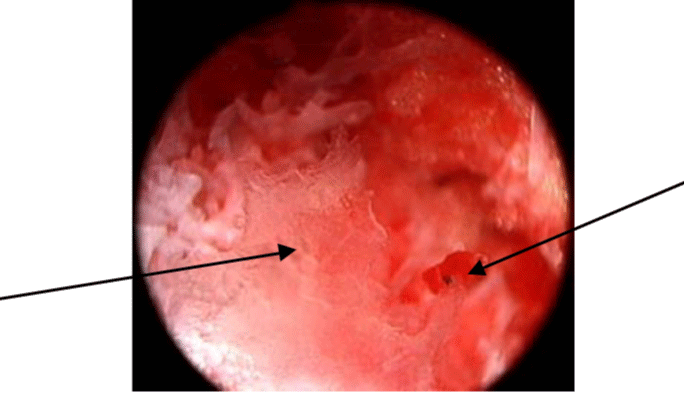
An osteoscopy of the inside of the osteoporotic right femoral neck was performed. As shown in the picture below, the cancellous bone has almost totally disappeared. Few adipocyte cells are seen along the walls [7] (Figure 2C).
Coral graft
In a second step, a natural coral filling-graft was performed. 15 gr of coral beads were grafted. Beads were 2,5 mm diameter.
Bone marrow
With a Mallarmé’s trocart, a sample of bone marrow was collected from the patient’s iliac crest, mixed with a few drops of heparin, used to fill in the coral beads. Then, the composite was placed in the gap of the femoral’s neck as shown in the pictures below.
Follow-up
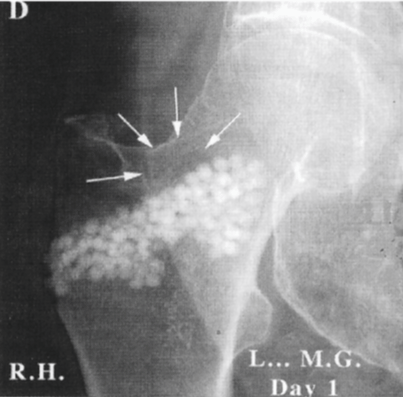
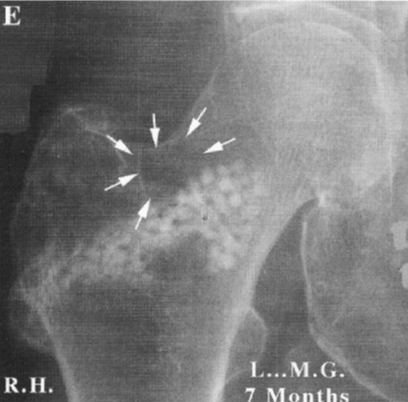
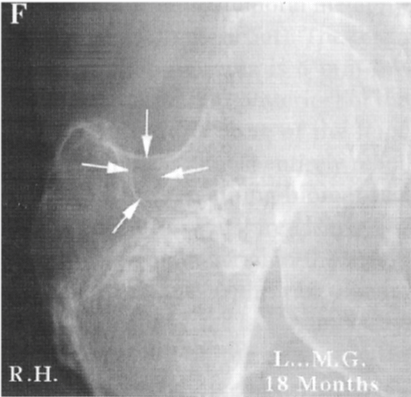
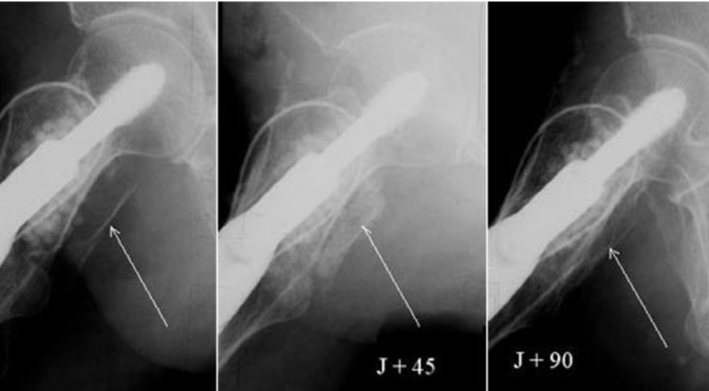
X-Rays below show the gradual disappearance of natural coral on a visual scale (Figure 2D-F).
Figure 2F: 18 months follow-up. The coral graft has almost totaly disappeared to be replaced by bone.
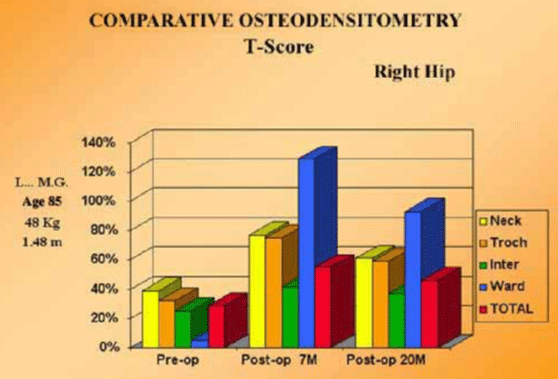
Post-operative densitometry (10) (Figure 3)
The post-operative osteodensitometry shows major reconstruction of the bone structure with a 20% increase in the high-risk zone (Ward’s triangle) 7 months after surgery, and 18 months after surgery the mineralization is almost 80%. A question remains: why 7 months after graft the intertrochanteric densitometry is so high in the Ward’s Area: more than 120%? Normally, it is impossible to get more than 100 % of the normal physiological amount. The 120% is due to the sum of the calcium in the femoral neck (walls and lamellae), plus the remaining natural coral; and, at last, the new bone formed. 20 months later, as it is shown below, the decreasing percentage of new bone in all analyzed sites supports this analysis [9-12].
Clinical Results
Clinically, two years and a half after the graft, this patient could leave her home again, did her shopping with her daughter and visited the supermarket. She danced at Christmas with her grandson. At her last clinical examination, she had gained 15 kilos and was in good health. Mentally, her life had been transformed.
The graft of biomaterial, restored the strength of her bone structures, allowing this patient to regain full autonomy and to overcome fear of falling generally observed in patients who suffered a previous fractured hip.
Being able to stand up is a major factor for the well-being, particularly for the elderly, as well as helping them conquer their fear of falling, avoiding severe sequelae for the time they have left to live.
Biological natural coral properties
Conventional x-rays
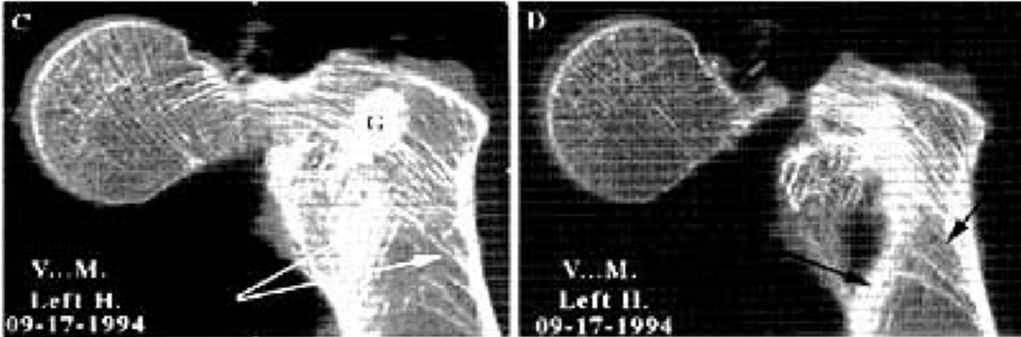
The coral (porites) has been chosen because of it’s natural properties, as it is bioresorbable, as seen on the Xray of the young patient below (Figure 4).
NMR
On the NMR below, it is impossible to distinguish the implanted zone from the non implanted bone in the spongy bone femur after disappearance of the biomaterial. (Figure 5AB).
Scanner
Note the size of the bony void, the complete disappearance of bone trabeculae. The remaining bone trabeculae is the site of microfractures (arrows on left slide) which have been described by Maurice Michel Forest (Figure 6AB).
Note the partial persistence of the coral graft (G: on left slide). The bone reconstruction with redevelopment of good arched trabecular, characteristic of the anatomy of the upper end of the femur. The cuts are made each 2,5 mms (Figure 6CD).
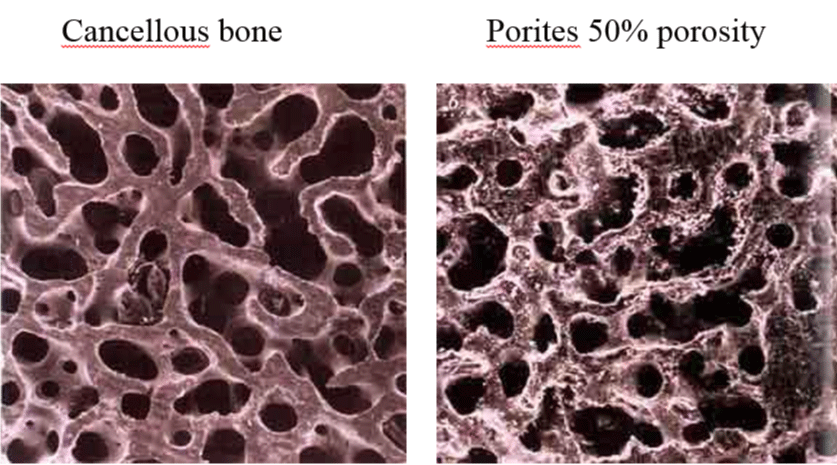
Physical properties
This material, of natural origin, is a pure calcium carbonate (98%) compound in its crystalline phase: aragonite. It displays great architectural regularity, with open pores allowing fluids to circulate freely inside the skeleton. The open pore porosity of Porites is 50%, which is similar to the cancellous bone [13-15] (Figure 7).
This porosity varies according to the species of coral under consideration. Once implanted in bone tissue, the volume of porosity, pore interconnection, regularity and diameter (150 µm on average) produce a total and rapid invasion of the graft by blood or bone marrow cells, as soon as vascularization is established. The coral architecture provides an exceptional surface for exchanges between the biomaterial and the bone.
Corals are essentially composed of mineral elements but also several appropriate amino acids – which should be eliminated, or at least reduced as much as possible - using specific purification processes such as supercritical fluids – to avoid, minimize and/or remove any harmful immune reactions.
There are differences between coral and fresh bone. The mineral phase in particular – 2/3 of bone composition – which is essentially in the form of calcium phosphate. Although the organic phase is important in bone – 1/3 of its composition – it is reduced to a very small proportion of amino acids in coral [16-18].
There are analogies: Two have specific action. Strontium is involved in the growth of bone crystal. Fluorine increases bone formation in spongy bone, in small doses and has the opposite effect on the bone walls at high concentration. It acts by stimulating osteoblast precursor cells.
Osteoscopy
There are non-functional vessels, as in any vascular structure. These vessels could be opened to increase blood flow, particularly under mechanical stress. There are functional vessels on the surface of the bone lamellae, along the edges and on the surfaces, carrying blood elements. They are only a few microns apart (approx. 12). These arterial and venous capillaries are very small in diameter and only allow the circulation of one cell visible to the naked eye [17]. There are larger arteries which beat to the rhythm of the pulse. Brown masses can be seen in the shape of vessels and these look like to micro-thromboses (Figure 8).
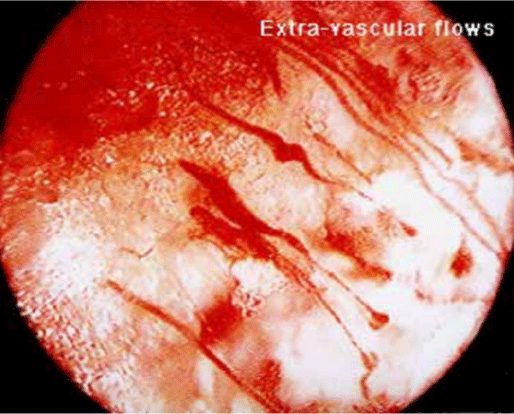
Blood can be seen to flow in the metaphyseal space at a regular rate and continuously, from small diameter vessels (Figures 9,10).
Figure 8: Osteoscopic view of an osteoporotic upper femoral metaphysis. Demineralised plates (left arrow); Possible Microthrombosis (right arrow).
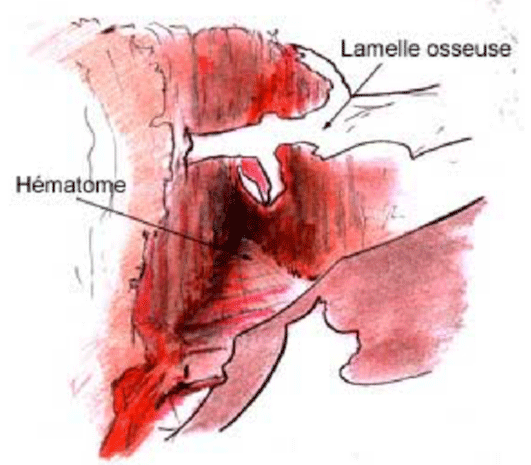
Pathological blood flows in the metaphyseal upper femoral neck
Haematoma can be seen inside the pathological bone.
Rigid bony plates can be seen and other which are partly rigid and partly flexible. Bone lamellae can be seen, parallel to each other, forming a kind of orderly architecture. Detached bone lamellae can be seen, distributed chaotically. Orthogonally shaped plates can be seen on all four sides. Some have the same transparency or opacity, others contain a clearer oval shape. Some are homogeneous throughout, others are clearer at some points. Some are solid, others are perforated [19]. The hole is in the centre or along the edge of the plate. Certain lamellae have parallel edges, others are swollen in the middle. Some are attached to each other, others are separated and float freely [20].
There are compact masses of adipocit cells. In other places, there are isolated sprinking like glorious golden beads in the optical field. All the bone lamellae are white and remain so.
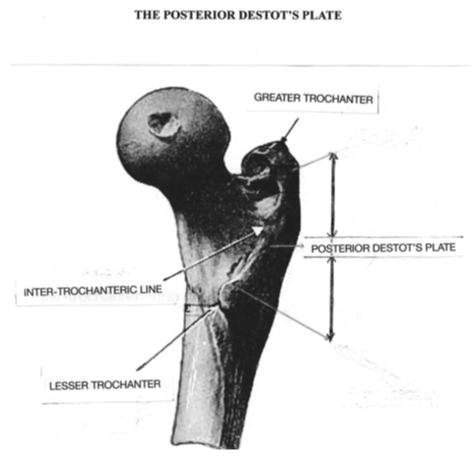
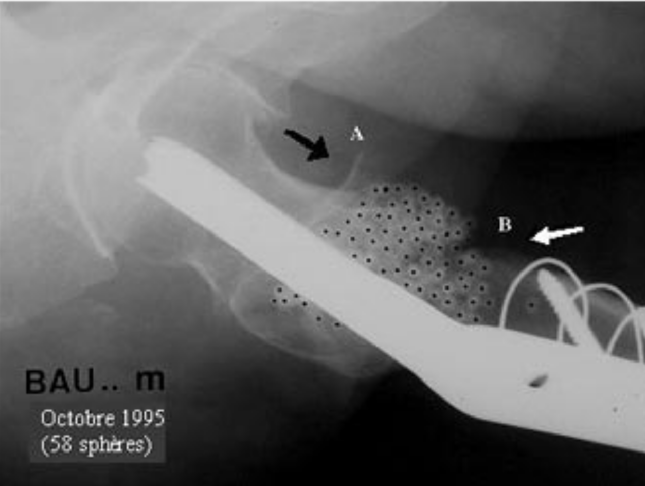
Incredible reconstruction of destot’s posterior plate
When the posterior inter-trochanteric plate describes by Destot is broken either in one ou more fragments, nobody can rebuilt it by a mechanical mean. So, although it is a major piece for the broken hip’s stabilization, nobody takes care of it. The biocoral can do it (Figure 11).
First case
The posterior plate is broken in one big fragment. 90 days after it is anatomically in place (Figure 12).
Figure 12: The posterior plate is broken in one big fragment. 90 days after it is anatomically in place.
Second case
This is the extraordinary possibility of natural coral to rebuild a bone by a biological process similar to the natural bone metabolism (Figures 13,14).
Functional hypothesis
Small vessels may suffer necrosis. The interruption of the blood flow may be due to microthromboses, flexibility of plates may be due to the chemical release of mineral ions. The black spots seen in many X-ray samples may be due to micro-thromboses. Is the destruction of mineral plates only due to cell destruction? Beyond a certain stage, aren’t the proteolytic elements of haematomas involved in this process? Don’t haematomas play a part in the pain patients suffer after prolonged walk because of the hyper pressure inside the bone? Are bone lamellae of different shapes separated from each other simply by chemical phenomena (rupture at the end of the chain) and/or due to mechanical phenomena (such as fatigue microfractures)? Does the swollen shape of certain lamellae reflect the microfractures described by Maurice-Michel Forest?
We must rely on fundamental research to explain to us what cannot be understood. When such a high degree of bone destruction is attained, no drug is able to enter the bone and treat the disease except when placed in situ [15,16].
The solution is here. Filling empty spaces, using a compatible, strong material which will act as a vector, rebuilding vessels and cells carrier, which the bone needs for its reconstruction. At the same time, they must rebuilt the anatomy, i.e. minimise as much as possible the sequelae which will inevitably occur if they forget to treat all secondary fracture lines. The coral in the cancellous missing bone acts exactly as the natural normal bone. This is the gift of nature.
What a challenge we must hope that our colleagues, particularly the young ones, become aware that the elderly are our historical memory and it is a duty to thank them for it. What better gift could we give them than restoring their autonomy for as long as possible?
Discussion
Natural coral after an excess of honor reached the shallows of oblivion. History has shown that once something hit the bottom it can take years - if ever - to reach its previous highs. If it is sure that the coral is the best biomaterial in the world, what happened then? Why this oblivion? The reason is that some immunologic reactions came in some very particular cases when and where a big piece of coral was used, equal or larger than 1 cm thickness. These reactions were seen in the correction of a 10 or more degrees genu varum deviation. Nothing happened when using small pieces under 5 degrees and with beads of 2 to 3 mm of diameter, not any case of immunologic reaction was seen. Some proteins may have been left in the big specimen due to an insufficient purification. When the supercritical fluid technic was used, the remaining protein molecules in the heart of the aragonite cristal were removed. No more immunologic reactions were described later on. Unfortunately, it happens too late. The surgeons recall only the failure and do not try to know what was the scientifically reason the damage was done Exit the coral what a pity.
Conclusion
Osteoporosis is today’s disease. “As a watchman waits for dawn”, so we observe the hours, days, months and years go by. We wait. What are we waiting for to decide to solve this problem? We already hold the cards. Defining the populations at risk? We know them. Define osteoporosis?
We know it. Can we detect the risks? We know them. Can we treat the complications? We know how.
It is often said that “the elderly do not contribute to society”. Are we so sure? They have experience of life, of their profession; they have professional qualifications which may be useful one day and are sometimes irreplaceable. They can look after children. In any case they have made and pay their contribution to society. Sometimes they have paid a heavy “tribute” to it.
Our duty and honour is to acknowledge what we owe them, and through natural generosity, help them to negotiate the final stretch under the best possible conditions.
The majority of people live in permanent fear throughout their lives. We do not intend to list the fears and provide statistics – so beloved of technocrats. There is no point in saying that the first of them is fear of death. But how many other fears have to be overcome along the road Fear for one’s health, family, profession, relatives, friends, and pension. Finally, after overcoming all these trials one way or another, we arrive at the end of the road and the last hurdle is being unable to move around anymore.
Standing erect, man’s first acquisition, must be the last to disappear. You have to put yourself in the place of someone who has just fractured a hip. You have to know what she/he is suffering, not only physically, but intellectually, based on the terrible reputation of this fracture. Unfortunately this reputation is still valid today. We must not forget that there are still more than 70% of functional complications.
It has to be stated even more forcefully that this state of mind must change radically. We must affirm that this fracture should no longer have the sinister reputation it still carries. We are no longer in the age of the Gaul. Today, the most serious hip fractures can be treated with tremendous technical improvement. The bone stock must be restored on the one hand and the different parts of the fracture held in place on the other.
Today surgeons are in a fairly comfortable position. Because the patient is elderly, everyone waits fatalistically for the inevitable to occur. How many times do we hear “poor soul, she couldn’t stand the shock”. And the family is resigned to it.
No – this behaviour should not be accepted any more. Surgeons have technics which have proved their efficacy. They will benefit from the gratitude of the fractured patient and the thanks of the family. They will sleep easy, with the knowledge of a job well done. Is it not what all want?
Hip fracture should disappear forever when intrabone injection of bone substitutes will become a standard procedure, like breathing. This dream is within our grasp. Let’s dream together.
References
- The use of biocoral for hip fracture repair in ederly patients Biomineralization 93; 7th International Symposium on Bio mineralization; Monaco. 1993; 129-134.
- Cirotteau Y. Reconstruction des pertes de substances osseuses cotyloidiennes et fémorales lors des reprises de PTH à l’aide de corail naturel. Actualité en biomatériaux. 1993; 2: 179-187.
- Cirotteau Y. Upper femoral metaphysis morphological modifications of a human struck down by osteoporotic disease. Comptes Rendus de l'Académie des Sciences 1999; 401-411. Ref.:© https://tinyurl.com/y5vcz4et
- Patat JL, Cantaloube D, Cirotteau Y. Natural coral as bone graft substitute biomaterial. Corallo di ieri, corallo di oggi. Cultural heritage sciences and materials. European University Center for Cultural Heritage. RAVELLO. 1996; 2000. Ref.:
- Cirotteau Y. Behavior of natural coral in a human osteoporotic bone. Eur J Orthop. 2001; 11: 149 -160. Ref.: https://tinyurl.com/y24qu928
- Traum. Behavior of natural coral in a context of atrophic femoral non-union. Eur J Orthop.
- Treatment of bone diseases associated with demineralization of the bone. Official Health. Officiel Santé. SOFCOT 6/9. Nov 2006 ; 2 et 13 Ref.:
- Cornell CN. Management of fractures in patients with osteoporosis. Orthop Clinical North. 1990; 125-141. Ref.: https://tinyurl.com/yyrjr35v
- Barrios C1, Broström LA, Stark A, Walheim G. Healing Complications after internal fixation of trochanteric hip fractures: The prognostic value of osteoporosis. J Orthop Trauma. 1993; 7: 438-442. Ref.: https://tinyurl.com/yyd647tl
- Laval-Jeantet AM, Bergot C. Quantitative imaging and absortiometry of bone in aging. Cahiers of Anthropology and Human Biometry. 13: 263-280.
- Patel A, Honnart F, Guillemin G, Patat JL. Use of skeletal madrepore fragments in orthopaedic and reconstructive surgery. Calcif Tis Int. 1980. 31(Suppl 108).
- Kehr PH, Graftiaux AG, Gosset F, Bencheikh K. Use of biocoral in cervical intersomatic grafting. Biomineralization 93, 7th international symposium on biominerial Monaco. 1993; 123-128.
- Ouhayoun JP, Isaahakian S, Patat JL, Shabana AHM, Guillemin G. Histological evaluationof natural coral skeleton as a rafting material in miniature swine mandible. J Materials Science. 1992; 3: 222-228 Ref.: https://tinyurl.com/yxhkw2cu
- Guillemin G. Madreporic materials in orthopedic surgery. Teaching Notes of the S.O.F.COT N ° 25 French Scientific Expansion (Ed) Paris. 1986; 91-100.
- Osteodensitometries are made by biphotonic absorptiometry with no danger of radiation by the use of microcosmes. Hologic QDR-1000/W (S/N 851). They are performed by C. Bergot MD. Service of radiology; Pr Laval-Jeantet MD, Head of Service, Saint-Louis Hospital, Paris.
- All soft issues are removed; The simples are embedded in a wet sheet and put under the machine (80 KV- 100 mA) in a frontal plane. 20 cuts, every 1,5 mm, are made from the anterior (1) to the posterior (20) side of both samples.
- Cirotteau Y. A physiological approach in stabilization and consolidation of unstable femoral neck fracture in osteoporotic patients - A retrospective review. 2003; 13: 145-155. Ref.: https://tinyurl.com/y57uk3qm
- Cirotteau Y. Screw-plate angulation of 130° or 135° and 120° in the stabilization of an unstable trochanteric femoral neck fracture 2003; Eur J Orthop Surg Traumatol. 2003; 13: 173-178. Ref.: https://tinyurl.com/y3l3sutv
- Cirotteau Y. Boyd HB, Griffin LL. Classification: A refinement proposal. Eur J Orthop Surg Traumatol. 2002; 12: 152-157. Ref.: https://tinyurl.com/y3wbzt7d
- Sacks O. The man who took his wife for a hat. Editions du Seuil. 1988; Ref.: https://tinyurl.com/y5y3qzl7